Intensive Care Medicine
@yourICM
International peer-reviewed medical journal for all involved in Intensive Care #FOAMed #FOAMcc
🖋 Write https://t.co/j4p0oZF5XA
📨 Submit https://t.co/BJMsQ4rNz3
ID:1011605395
https://www.springer.com/journal/134 14-12-2012 17:33:14
5,6K Tweets
70,7K Followers
156 Following
Follow People


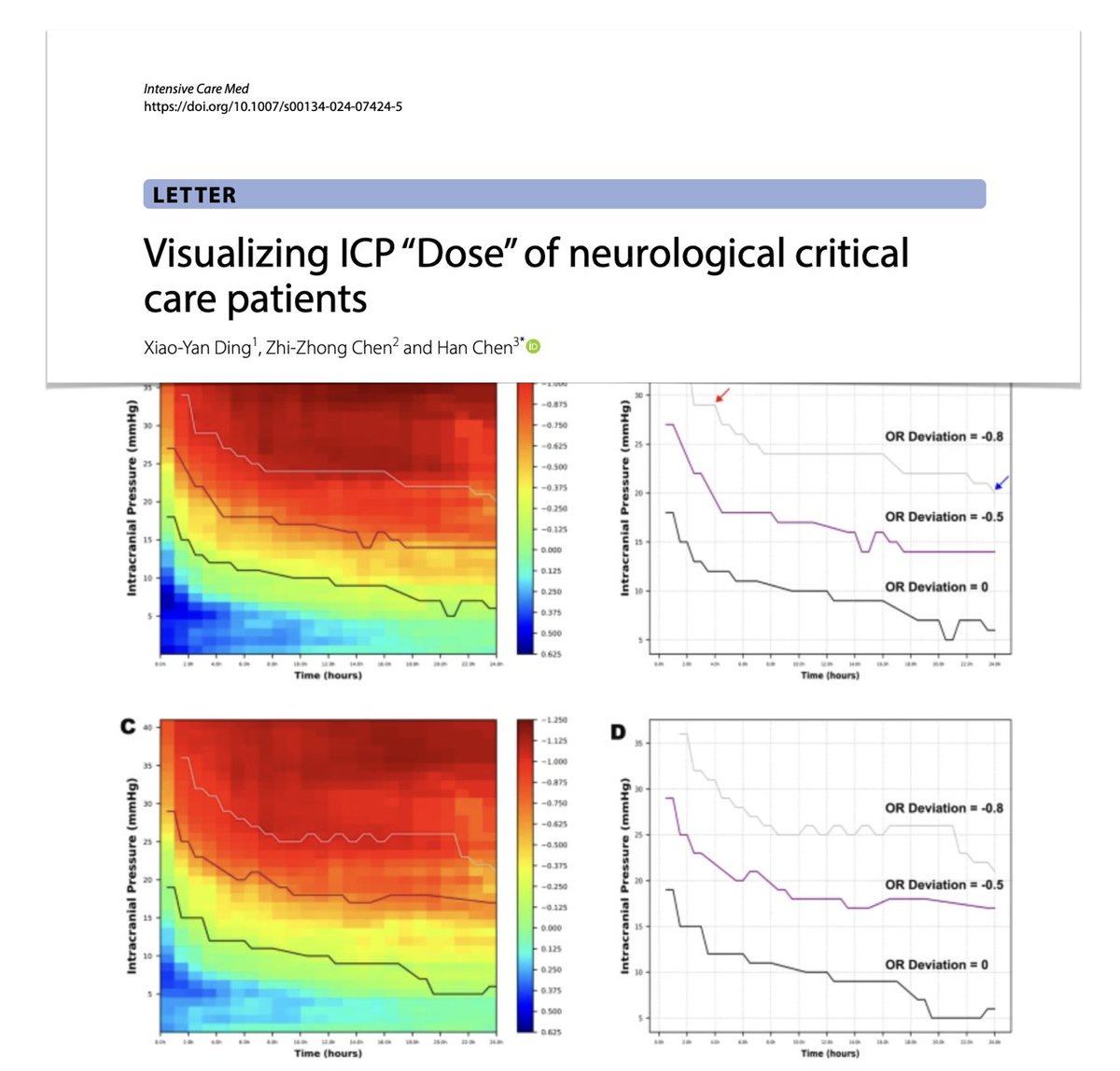
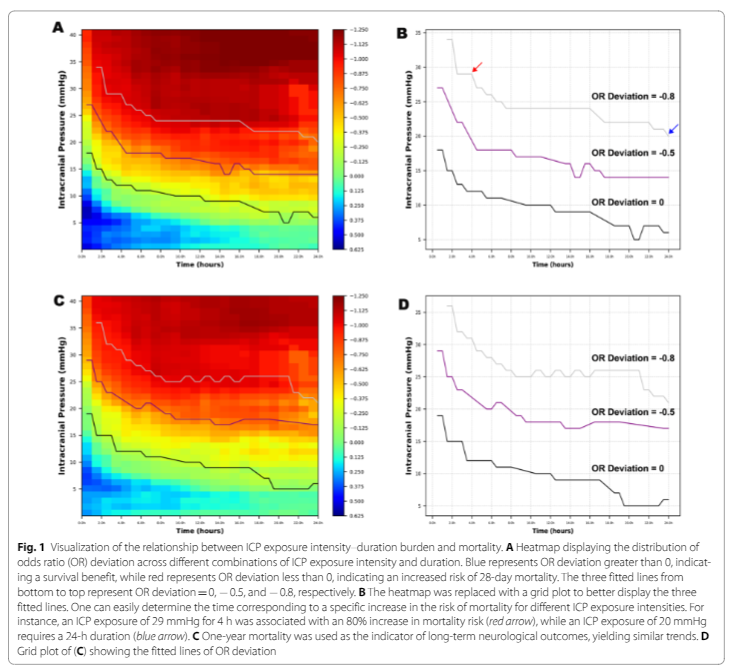
So happy to see our paper on ICP dose published in Intensive Care Medicine in 2015 (!) being reproduced once again - ICP toxicity is about dose, not about crossing a threshold Fabian Güiza
doi.org/10.1007/s00134…




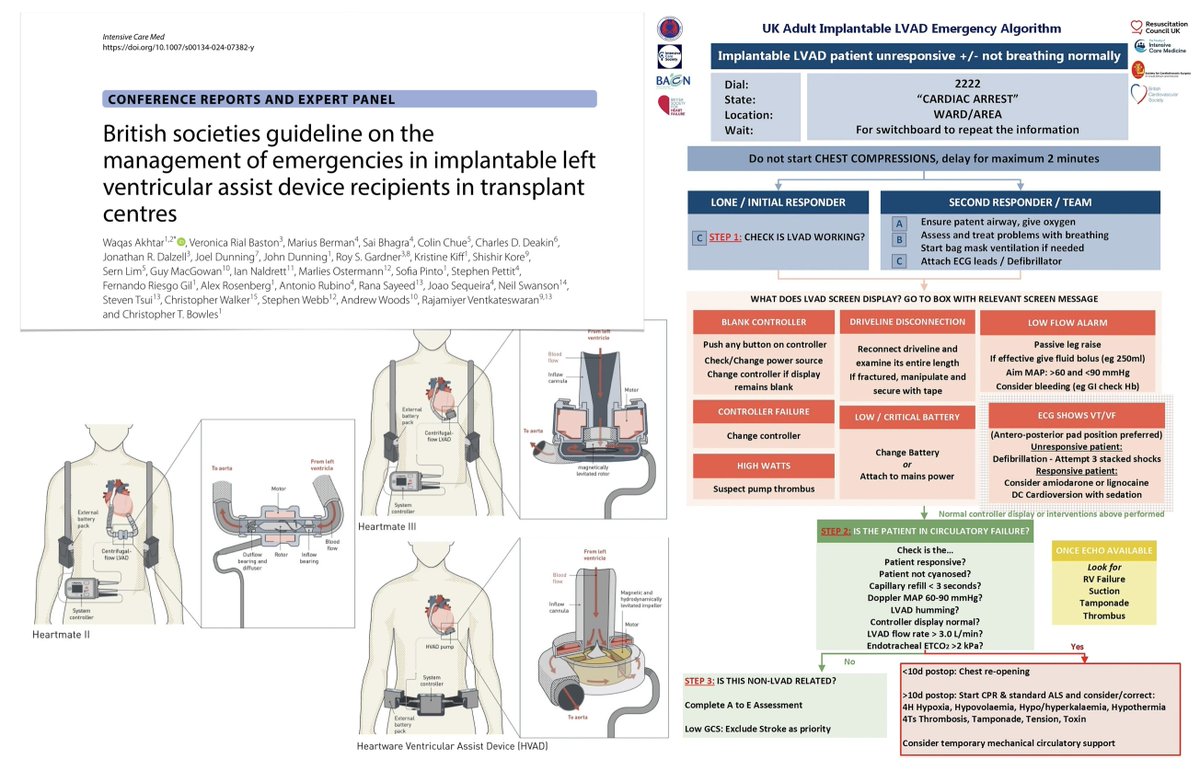
How to manage emergencies in #LVAD recipients in #transplant centres?? British societies guideline #FOAMcc on Intensive Care Medicine
🇬🇧UK emergency algorithm development
⏱️initial response & initial/secondary responder
⚙️ #troubleshooting
🩸adequacy of circulation
🔓bit.ly/4ae1xus

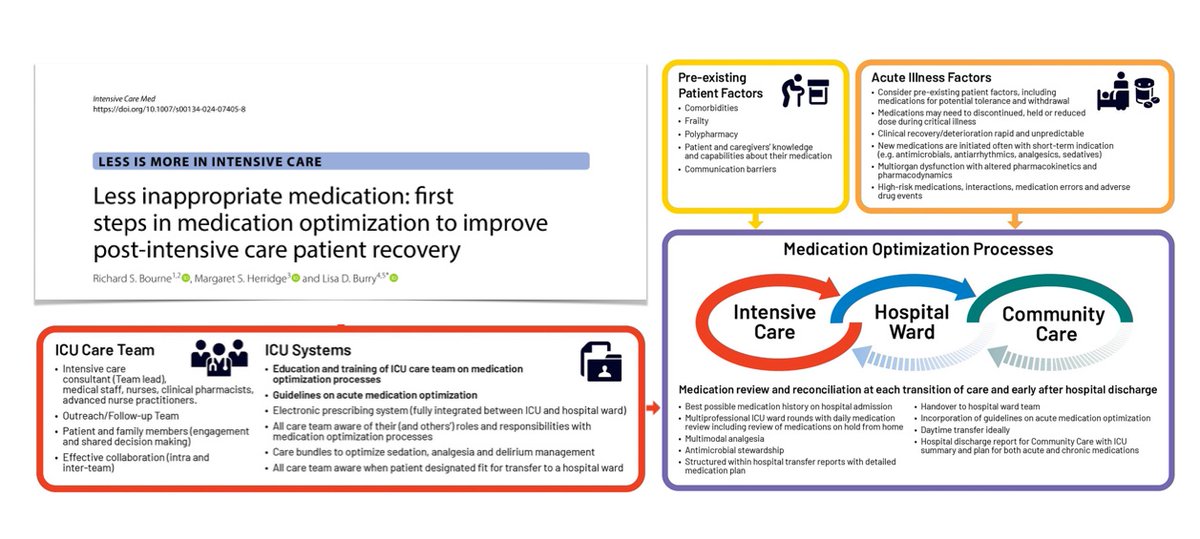
Intensive Care Medicine 4/🔹Less inappropriate medication: first steps in medication optimization to improve post-intensive care patient recovery 👉rdcu.be/dFBvy
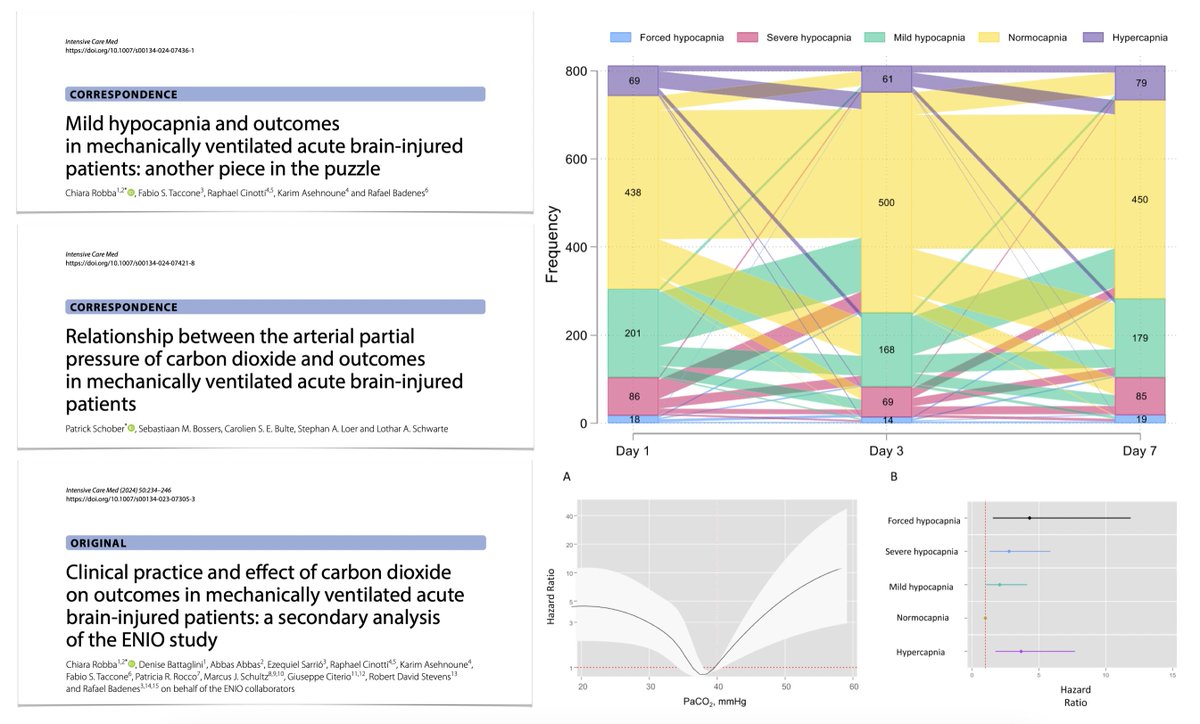
🔹Relationship between the arterial partial pressure of CO2 & outcomes in MV-acute brain injured patients 👉 rdcu.be/dFBuW


1/ Intensive Care Medicine's highlights:
🔹Visualizing ICP “Dose” of neurological critical care patients👉 rdcu.be/dFBuU
🔹Mild hypocapnia and outcomes in mechanically ventilated acute brain-injured patients: another piece in the puzzle 👉 rdcu.be/dFBuV



🧠I cannot agree more‼️ 🧐
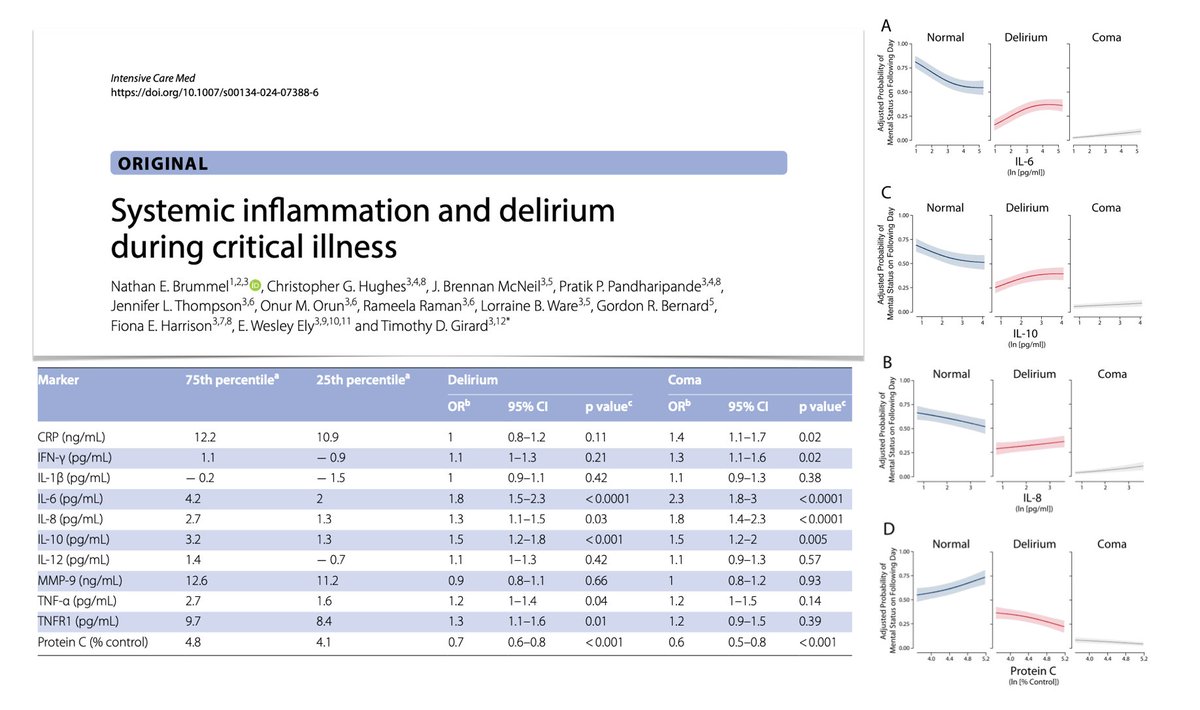
Systemic inflammation = DELIRIUM
In a study published in Intensive Care Medicine
⬆️ IL-6, IL-8, IL-10, TNF-α, TNFR1 and ⬇️ protein C were associated with ICU delirium. WesElyMD
We have shown this with other markers
pubmed.ncbi.nlm.nih.gov/31684066/
pubmed.ncbi.nlm.nih.gov/31336587/


1/ Intensive Care Medicine's latest manuscripts of the topical collection 'ICU Toolbox':
🔹Monitoring esophageal pressure 👉 rdcu.be/dE18u
🔹Management of the brain-dead donor in the intensive care unit 👉 rdcu.be/dE18i




#ICMpn #OpenAccess
📢Have a look at what your peers are reading most.
A selection of most influential papers
rb.gy/wvh2wr
#neonates #criticalcare #Furosemide #kidneyInjury #premature #oxygentherapy #bronchiolitis #sepsis
More contents at rb.gy/ycnkql